The Problem
Maine is in the midst of a dental health crisis. If you’re just learning this for the first time, that might sound like a startling statement. And if you’ve known that for some time, you might be wondering why it is still true. Many factors contribute to this crisis, and two of the biggest factors are a lack of awareness about the severity and scale, and the resulting lack of an appropriate, coordinated response. Tooth decay, also called caries and more commonly known as cavities, impacts more children than allergies and asthma, though it does not get nearly as much public attention. Nationally, we have data through 2016 which indicates that of children ages 2-5, 23.2% have caries in their primary teeth. By third grade, 44.7% of children in Maine have experienced dental disease. Finding oral health care services has been more challenging post-pandemic, and Maine no longer has a surveillance system to track dental disease in children. The situation has never been good, and the pandemic only made oral health challenges worse.
Oral health contributes directly to overall health. There is a pervasive misunderstanding of this critical interconnection, which has been reinforced by a legacy of siloing dental health from broader health care. Dental disease is the most common chronic disease of childhood, and yet neither the dental health system nor the primary care system treat it as such. It cannot be prevented exclusively with brushing and flossing; once a child is exposed to the bacteria that causes cavities (often from a caregiver), only tools that are accessible through a health care professional can truly prevent the disease from setting in or stop it in its early stages. Unfortunately, too many children in Maine go without any dental care.
Data: Difference between # of kids with a medical home vs dental home (can see the problem and opportunity – we can impact the number of kids getting oral health care in a medical home), # of kids getting oral health services in medical settings
Data:
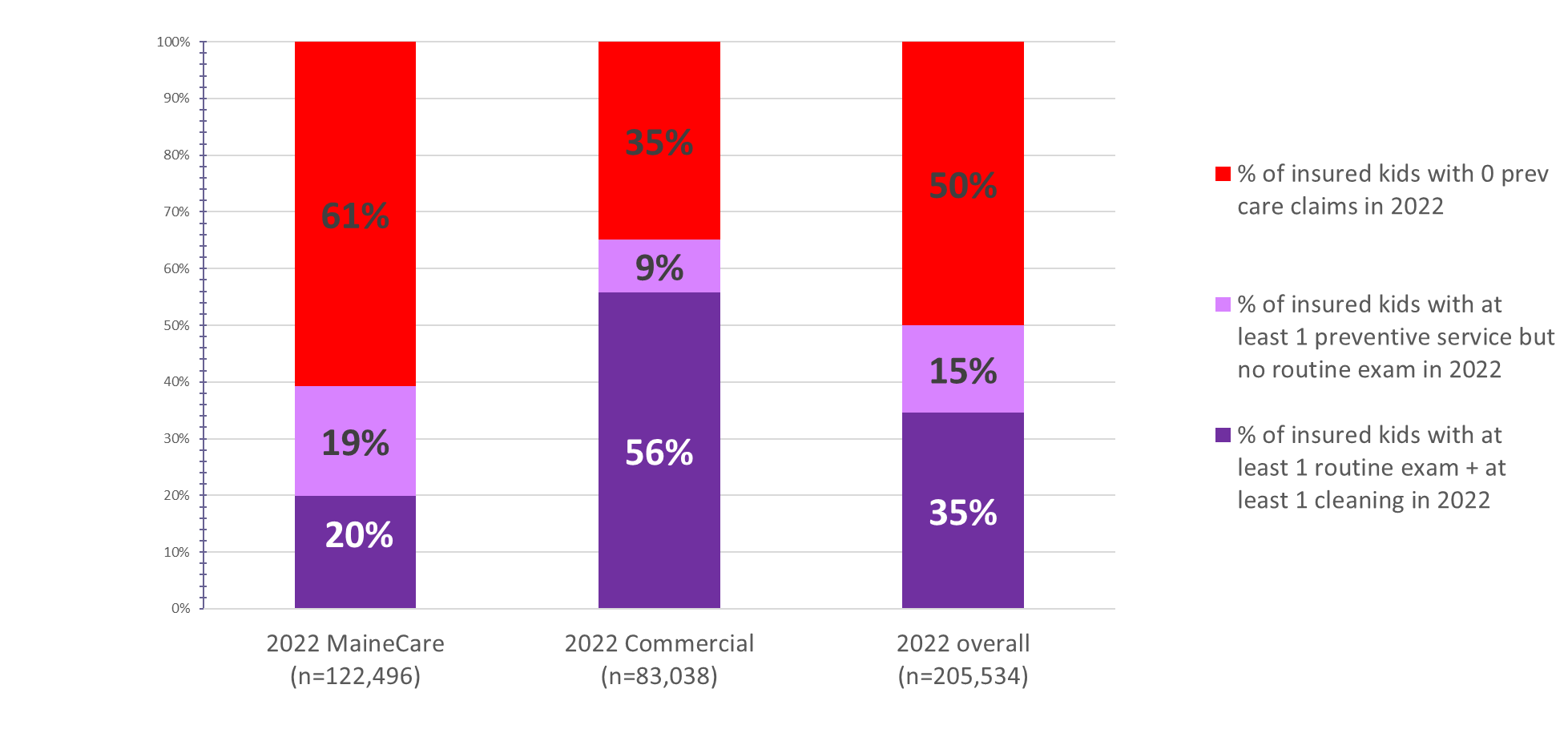
TO BE FOUND? # of kids receiving a preventive svc by ins type, from data brief
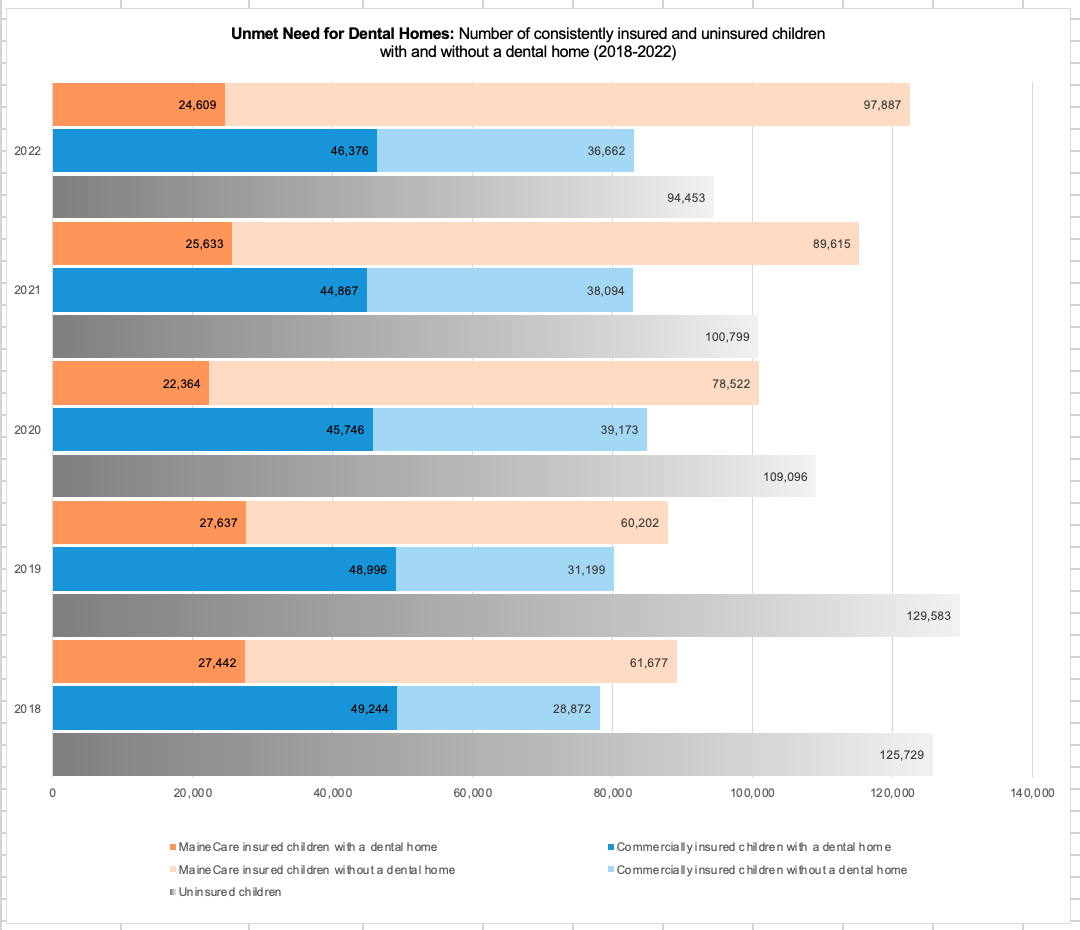
Stacked graph with kids who don’t have coverage or intermittent coverage, kids who have consistent insurance, kids who got any preventive services, kids who had active dental home (exam + cleaning)The design of the traditional dental system exacerbates the impacts of systemic racism, discrimination, poverty, and other disparities in access to care and therefore oral health outcomes. Because the system was built primarily on a for-profit model, private practice dentists are not required to serve people with public insurance or people who are uninsured. People with public insurance or who are uninsured are more likely to identify as a person of color, as having a disability, as having low income, and/or as a member of another socially marginalized group. Without specific interventions designed to bring oral health care to these people, they will continue to fall behind in terms of oral health care access and outcomes.
Trackable: MaineCare utilization dashboard (race, language), demographics of Medicaid recipients
More static: Because there is less data available on oral health disparities, especially in Maine, COHN supports organizations working directly with people facing systemic discrimination to better understand their oral health challenges. You can find equity profiles and other relevant source materials on our Equity and Data pages. (pull from equity profiles: DRME, foster care, NPMHI, others)
We must use our better and more comprehensive understanding of dental disease to inform solutions for treating and managing it as a chronic disease. New technology allows us to avoid drilling-and-filling by treating caries like a chronic disease and managing lesions using minimally invasive care with new products like silver diamine fluoride, glass ionomer, povidone iodine, and more. This type of care does not necessarily fit into a “twice a year” dental visit model though it provides opportunities for more high-quality care to be delivered in community settings by a wider array of health care professionals.
Data:
# Application of SDF in dental claims,
# glass ionomer (2940),
# temporary restorations,
# povidone iodine?,
# OR cases,
# ER cases (DQA measure),
# SDF in primary care settings (likely only MaineCare data for a while)
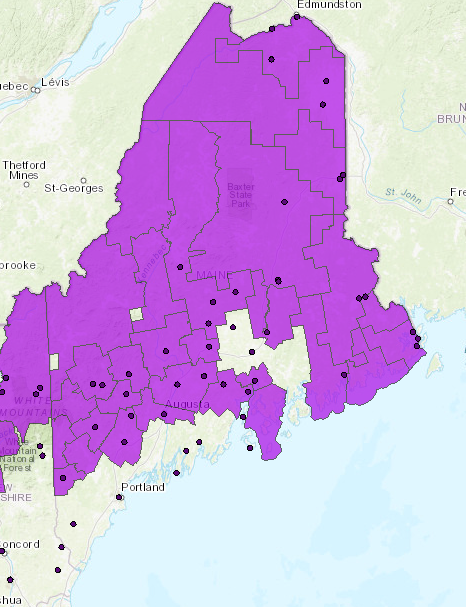
Expanding and diversifying the dental workforce will ensure delivery of community-based and minimally invasive care at the scale needed to serve all Maine children. There is a dental workforce shortage, and there are currently not enough dentists and hygienists to serve all people in the state with the traditional model of dental care, let alone providers trained in providing minimally invasive care in community settings. In addition to a long-standing dental workforce shortage, there are policy limitations with both public and private insurance that hinder the ability to provide care in community settings and to use the techniques we know are best for maintaining oral health. The workforce data also clearly demonstrate that relying primarily on dentists providing care in the traditional dental home model won’t solve this problem.
Data:
Dental HPSA data: https://data.hrsa.gov/maps/quick-maps?config=mapconfig/HPSADC.json:
age of people with dental licenses (if we can get from MDA/BDP?)
# licensed hygienists with PHS and/or IPDH status (Licensing dashboard)
There is insufficient infrastructure within state government to support strategies to address oral health as a public health issue. Maine only recently restored one permanent staff position at the Maine Center for Disease Control to lead public oral health efforts. MaineCare, the state’s Medicaid program, does not have a dental director, yet the majority of Maine children with consistent dental insurance (41%) are covered by MaineCare. Without sufficient staffing to address issues specific to oral health within the scope of these agencies, these issues persist and grow.
Data:
# full time (permanent) staff at Maine CDC: 1
# oral health staff at MaineCare: 0
Funding for these oral health at the state
Active oral health surveillance system within the Maine CDC: 0*
*Surveillance data from Maine CDC
2019 MIYHS (has large confidence intervals, parent self-report)
2012 report
